At UVISA Health, we want to understand the challenges healthcare professionals face when treating vulvovaginal infections. So we surveyed and interviewed 36 practitioners – including GPs, sexual health doctors, gynaecologists, pharmacists, and women's health specialists – to hear their honest thoughts about current treatments. What they told us was eye-opening. And concerning.
A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
At UVISA Health, we want to understand the challenges healthcare professionals face when treating vulvovaginal infections. So we surveyed and interviewed 36 practitioners – including GPs, sexual health doctors, gynaecologists, pharmacists, and women's health specialists – to hear their honest thoughts about current treatments. What they told us was eye-opening. And concerning.
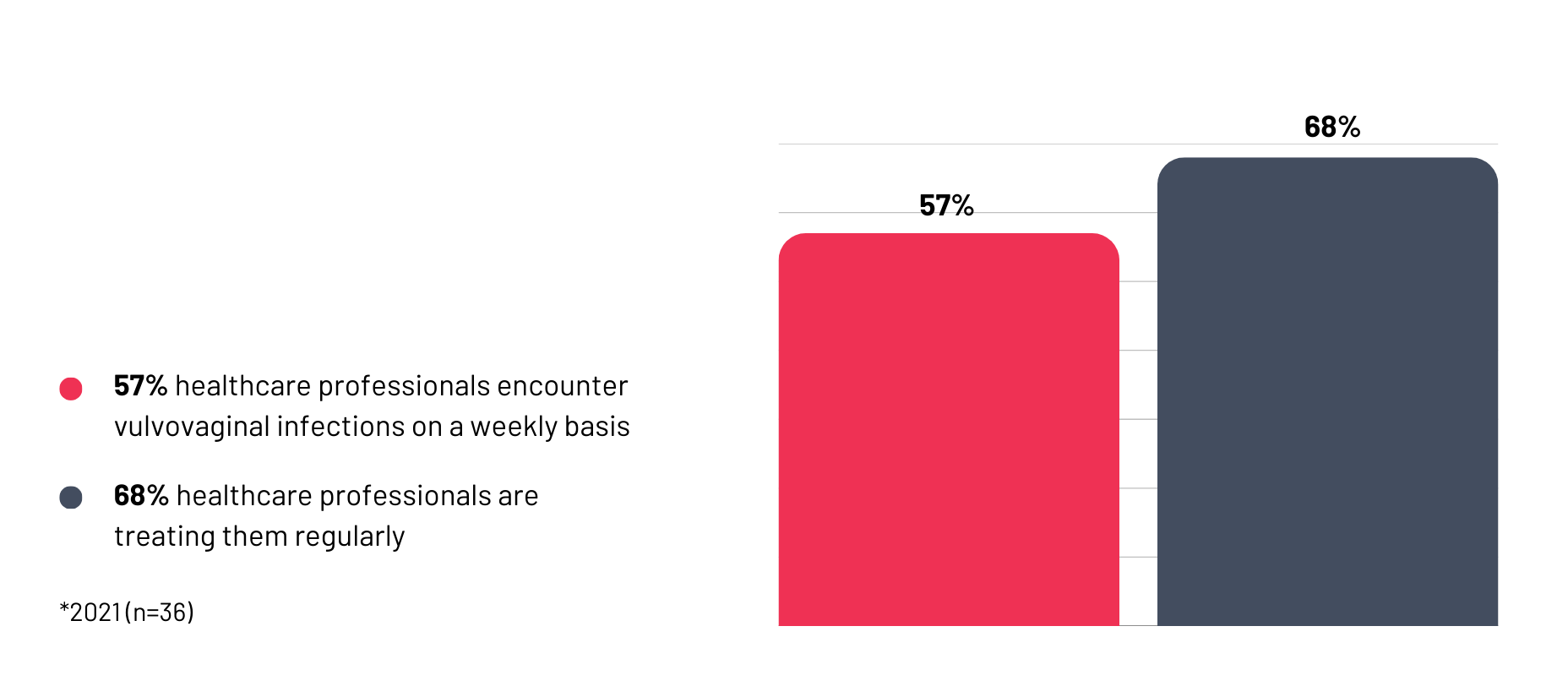
Among our surveyed professionals, 57% encounter patients with vulvovaginal infections weekly, with 68% treating them regularly. The impact of these infections spread far beyond physical symptoms – disrupting sleep, relationships, and work performance.
What's particularly troubling is how much suffering remains hidden. Especially since the pandemic, women have increasingly turned to self-management, taking self-swabs and cycling between different pharmacies when symptoms persist. That suggests healthcare professionals are only seeing the tip of the iceberg and those cases where over-the-counter solutions have repeatedly failed.
‘We see women who become high healthcare service users, repeatedly coming to see their doctor for help,’ explains one doctor, describing patients trapped in cycles of temporary relief followed by recurrent infection.
This was the stark assessment from all healthcare professionals when discussing current antibiotic treatments for bacterial vaginosis. Their concerns are multi-layered and deeply troubling.
The immediate problem is side effects and microbiome damage. Antibiotics don't just target harmful bacteria – they destroy any good bacteria present that may help restore the vaginal microbiome. Repeat antibiotic treatment for recurrent bacterial vaginosis, thus leads to women experiencing recurrent thrush following the antibiotic treatments.
The psychological impact is devastating, according to our data. Patients often express, ‘something is wrong with my vagina’, a belief that erodes their confidence and sexual wellbeing, effects healthcare professionals witness every day..
As the gut microbiome is disrupted with antibiotics, diarrhoea and bloating are common side effects too. And it can take weeks for women to feel back to normal after completing treatment, leading them to feel frustrated with this solution and often discontinuing the treatment with first signs of temporary relief.
Beyond individual patients, there's a global crisis brewing. Pharmacists, who take their ‘Antibiotic Steward’ role seriously, have noticed alarming increases in antibiotic prescribing since the post-pandemic shift to virtual consultations. As one healthcare practitioner put it, in overwhelmed clinics ‘the easiest way to end a consultation is to prescribe antibiotics.’
All of this contributes to antimicrobial resistance: a global crisis pharmacists see firsthand, as they serve multiple GP practices and witness daily antibiotic usage across their communities.
The message from our survey respondents is clear: they clearly want change in the way vulvovaginal infections are treated. 100% expressed interest in alternatives to current options. And 96% said they would recommend a clinically proven light therapy device for vulvovaginal infections.

For that to happen, doctors told us they want to see clinical evidence of safety and effectiveness, no negative impact on the vaginal microbiome, competitive pricing, and ease of use. What truly matters to them is not that it’s cheaper than current options, but delivering an effective treatment that protects the good microbiome; something current options fail to do..
When asking about the delivery of a new treatment option to patients, a third of the healthcare practitioners would be comfortable with GP prescription, while 29% prefer over-the-counter availability following a pharmacist consultation – similar to the current approach used for bacterial vaginosis and thrush treatments in the UK.
Crucially, they felt uneasy with non-pharmacy selling, believing medical oversight is essential.
If you're struggling with recurrent vulvovaginal infections, these findings validate what you already know: current treatments aren't working well enough. Healthcare professionals understand your frustration and want better options too.
While we continue developing our light therapy solution, here's what you can do:
Don't suffer in silence. Our survey revealed a hidden burden, but healthcare professionals want to help. If over-the-counter treatments aren't working, see your GP.
Track your symptoms. Understanding patterns may identify triggers you can avoid and can help healthcare professionals provide better care..
Ask questions. Don't hesitate to discuss and talk openly about concerns, including antibiotic side effects.
Our survey shows that healthcare professionals desperately want better treatment options, but current solutions are failing both practitioners and patients.
Alternatives are needed that don't disrupt the microbiome, don't contribute to antimicrobial resistance, and that work for recurrent infections. Women need treatments that end the cycle of temporary relief and recurring symptoms.
That's exactly what we're building – a clinically proven light therapy device that helps women and healthcare professionals.
We will continue to:
Do you want to be part of the change? Our survey is still live. Share your story and help us shape a real, lasting solution.